Existing Models of Maternal Death Surveillance Systems Protocol for a Scoping Review
- Research article
- Open Access
- Published:
Evaluation of the Maternal Death Surveillance and response organisation in Hwange District, Zimbabwe, 2017
BMC Pregnancy and Childbirth volume 19, Article number:103 (2019) Cite this commodity
Abstract
Background
Maternal Death Surveillance and Response (MDSR) system was established to provide information that finer guides actions to eliminate preventable maternal bloodshed. In 2016, Hwange district sent six maternal death notification forms (MDNF) to the province without maternal decease audit reports. Timeliness of MDNF reaching the province is a claiming. Two MDNF for deaths that occurred in February and May 2016 just reached the provincial office in September 2016 meaning the MDNF were seven and four months late respectively. Nosotros evaluated the MDSR system in Hwange commune.
Methods
A descriptive cantankerous-sectional study was conducted. Wellness workers in the sampled facilities were interviewed using questionnaires. Resource availability was assessed through checklists. Epi Info 7 was used to calculate frequencies, means and proportions.
Results
Nosotros recruited 36 respondents from 11 facilities, 72.2% were females. Inadequate health worker noesis, lack of induction on MDSR, unavailability of guidelines and notification forms and lack of knowledge on the flow of data in the system were reasons for late notification of maternal deaths. Workers trained in MDSR were 83.8%. Only 36.1% of respondents had completed an MDNF before. Respondents who used MDSR information at their level were 91.7%, and they reported that MDSR system was useful. Responsibility to complete the MDNF was placed on wellness workers. Maternal death case definitions were bachelor in 2/eleven facilities, 4/11 facilities had guidelines for maternal death audits. It costs $60.78 to notify a maternal death.
Determination
Reasons for tardily notification of maternal deaths were inadequate knowledge, lack of induction, unavailability of guidelines and notification forms at facilities. The MDSR system is useful, acceptable, flexible, unstable, reliable but non uncomplicated. Maternal case definitions and maternal death audit guidelines should be distributed to all facilities. Training of all wellness workers involved in MDSR is recommended.
Background
Maternal Death Surveillance and Response (MDSR) refers to continuous, systematic drove, analysis, estimation and broadcasting of information regarding maternal deaths. It links the health data system and quality improvement processes from local to national levels [1]. The Globe Health Organization (WHO) defines a maternal death, equally the decease of a woman while pregnant or within 42 days of termination of pregnancy. This is irrespective of the duration and the site of the pregnancy, from any crusade related to or aggravated past the pregnancy or its management but not from adventitious or incidental causes [2,three,4].
In 2015, the maternal mortality ratio was estimated at 216/100,000 live births globally [5]. This maternal mortality ratio translates to approximately 830 women dying every single day due to the complications of pregnancy and childbirth. Most all these deaths occurred in low resource settings, and virtually could accept been prevented [half dozen, 7]. The WHO African Region bore the highest burden with most ii-thirds of global maternal deaths occurring in the region [8]. The brunt is more pronounced in poor, rural areas where immature adolescents face a higher take a chance of complications and death as a result of pregnancy [ix]. In Zimbabwe, according to WHO the maternal mortality ratio was 614/100000 live births in 2014 [10]. The Millennium Evolution Goal (MDG) 5 of reducing the maternal bloodshed ratio to 71/100000 was far from being achieved [11]. Like many other developing nations, Zimbabwe failed to achieve the target for MDG v past 2015.
In the early 1990s, Republic of zimbabwe established a Maternal Mortality Surveillance and Response (MMSR) with the aim of providing data that effectively guides actions to eliminate preventable maternal mortality. In 2013 the proper name of the surveillance system was inverse to MDSR in line with the WHO guide of catastrophe preventable maternal mortality [12]. The Sustainable Development Goals proposed that progress toward ending preventable maternal deaths should continue to be measured by monitoring the Maternal Mortality Ratio [13]. When a maternal death occurs, three copies of the maternal decease notification form are completed, and i course is retained at the facility where the decease occurred. Ii forms are then transmitted to the district for capturing into the District Health Information Organisation (DHIS 2) then the two forms are sent to the province within 14 days of the expiry. At the province, the Provincial Maternal and Child Health Officer completes the relevant sections and retains one copy. The last copy of the grade is so submitted to the Reproductive Wellness unit of measurement at the caput office inside thirty days of the occurrence of a maternal death. Feedback is given at each level of the health care organisation [Fig. 1].
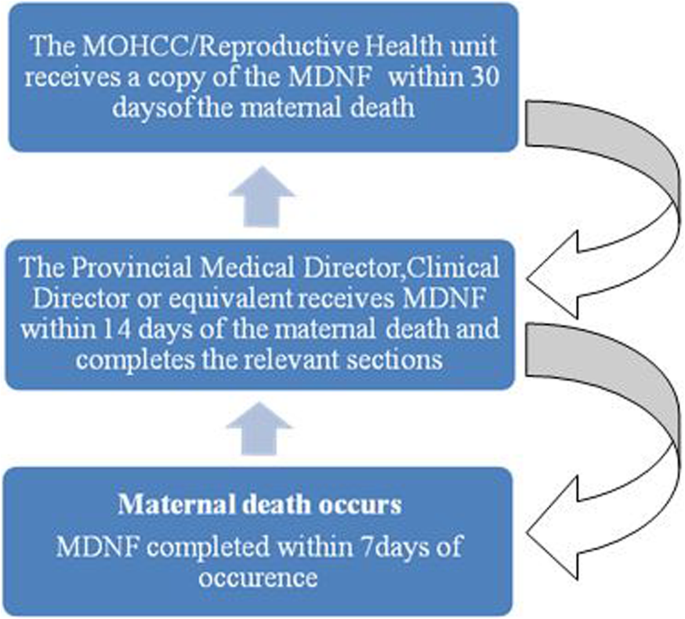
Current flow of the Maternal Decease Notification Course in Republic of zimbabwe
In 2016, Matabeleland N province recorded 24 maternal deaths compared to 17 deaths in 2015. Of the 24 deaths recorded, Hwange commune contributed ten, which is a third of all deaths in the province. Six maternal death notification forms from Hwange district that were sent to the provincial office were non accompanied past maternal death audit reports as per requirement. Timeliness of the maternal death notification forms reaching the provincial office was also a claiming. For ii maternal deaths that occurred in Hwange in February and May 2016, the forms only reached the provincial office in September 2016 meaning that the forms were 7and 4 months belatedly respectively. Deaths that are notified very late are often missed past the surveillance organization and missing maternal deaths creates a potential for seriously underestimating the magnitude of maternal mortality inside facilities. Information from the MDSR organisation is important in refining, targeting and ensuring efficient allocation of resources in the fight against maternal mortality. The study was conducted to evaluate the MDSRin Hwange commune in 2017.Specifically, we assessed wellness worker knowledge on MDSR, assessed the systems' usefulness and its attributes. We as well determined reasons for belatedly notification of maternal deaths in Hwange District, 2017.
Methods
Study blueprint
We conducted a descriptive cross-exclusive written report using the updated US Centers for Illness Control and Prevention guidelines for surveillance system evaluation in 2017 [xiv].
Written report setting
Hwange is one of the 7 districts in Matabeleland North province serviced by 22 health facilities, which include 4 hospitals, two urban clinics, 13 rural wellness facilities and three private surgeries. The district is situated in the south-western role of Republic of zimbabwe, and mining and tourism activities dominate information technology. According to the Republic of zimbabwe population demography of 2012, the population of Hwange district is 144,745.
Report population
The Provincial Maternal and Child Health Officer, Medical Superintendent, District Medical Officer, Customs Sister/District Nursing Officer were the key informants in the written report because they have in depth knowledge of what is going on in the community with regards to maternal health. The PMCHO is the overall accounting officer in the province as far equally maternal health is concerned. The Medical Superintendent is the overseer at Lukosi Rural hospital and communicates directly with the PMCHO. At commune level the DMO is in charge of the district. The Customs sis/ District Nursing Officer provides an entry betoken in terms of communication regarding maternal deaths from the Rural Health Centres. At facility level information technology is the responsibleness of the attention nurse to fill the Maternal Death Notification Course (MDNF) and reporting to the next level. Doctors, Nurses/Midwives and Primary Intendance Nurses were the primary respondents. All (due north = 10) maternal decease notification forms for 2016 were likewise reviewed. Maternal death inspect reports were also reviewed.
Sample size calculation
We used the Dobson's formula for calculating sample size for single proportions to calculate sample size.:
$$ \mathrm{north}=\frac{{\mathrm{z}}^ii\times \mathrm{p}\left(i\hbox{-} \mathrm{p}\correct)}{{\mathrm{d}}^2}. $$
where n = required sample size.
p = proportion of health workers with cognition on MDSR.
d = margin for error i.e. 10%.
Assuming that the timeliness of maternal deaths notified in less than 24 h from the occurrence of the expiry is 90% and a 10% compunction rate, a minimum sample size of 39 wellness care workers were interviewed. Due to the paucity of data on MDSR locally the sample size was calculated using a study by Urquiza et al. on MDSR in Mexico [15].
Sampling procedure
Hwange district has a total 22 health facilities that offer maternal services. Four of these facilities are hospitals which were purposively selected for the study because they provide different infirmary settings (urban government infirmary, rural authorities, mission hospital and a private hospital). Two facilities were urban clinics, of which but 1 was randomly selected. Four facilities were randomly selected from the rural commune quango clinics. The aforementioned method was used to select other health facilities. A total of 11 facilities participated in the study; at least two wellness workers from these facilities who were found on duty on the day of the interview were interviewed. A minimum of eight wellness workers in the maternity section on duty on the 24-hour interval of the interview were recruited into the study from the district hospital. From the mission infirmary, seven health workers on duty at the maternity department were also interviewed. From the remaining two private hospitals five health workers on duty were interviewed in each infirmary. Some of these facilities experienced maternal deaths during the flow under review, these included Victoria Falls hospital, Lukosi Rural Hospital and Hwange Colliery hospital.
Data collection techniques
We collected data on knowledge levels of health care workers on MDSR, assessed usefulness and attributes of the MDSR. Data for the study was collected by the researcher using newspaper based interviewer administered questionnaires. Information technology took on boilerplate about 15 to 20 min to administer the questionnaire. Information was entered manually. 112A checklist for resources availability was used to assess the stability of the arrangement. Maternal death notification forms of all the 10 deaths that occurred in Hwange Commune in 2016 were reviewed.
Pretesting of data collection tools
Nosotros pretested our data collection tools at Tsholotsho Infirmary, because the hospital provided a similar setting with the area under study. The sequence of the questions in the questionnaire was altered and then that the questions followed a logical sequence that made sense to respondents.
Data assay
We used Epi Info version 7 to compute frequencies, means and proportions.
Usefulness of the surveillance arrangement
Co-ordinate to the updated CDC guidelines for evaluation of surveillance systems, a public wellness surveillance arrangement is useful if it contributes to the prevention and control of agin health-related events, including an improved understanding of the implication of such events (fifteen). Respondents were asked what the data collected on maternal deaths was used for, and also what public health actions were taken based on the surveillance data. Minutes and reports of meetings held on MDSR were produced every bit bear witness.
System attributes
The definitions used for all the attributes assessed are from the CDC.
Simplicity
CDC defines simplicity of a public health surveillance system as both its construction and ease of performance while still coming together their objectives. This attribute was assessed past determining whether the implementers of the system have always filled any MDSR forms and too if they felt at that place is a need for them to be further trained in the practise.
Acceptability
Acceptability is the willingness of persons and organisations to participate in a surveillance system. Wellness care workers were asked whether they were willing to proceed participating in the MDSR. In improver, completeness and timeliness will likewise be assessed as a proxy of acceptability.
Stability
Stability is the reliability and availability of the surveillance system. Reliability is the ability to collect, manage and provide data properly without failure. Availability is the ability of a surveillance system to exist operational when it is needed. Stability of the MDSR was assessed by checking for consistency in reporting, availability of communication equipment and other textile resources needed for the surveillance system.
Timeliness
Timeliness refers to the speed at which data is transmitted betwixt dissimilar levels in the surveillance organisation. It was assessed by checking whether MDNF are completed within 7 days of a maternal decease and are so sent to the Provincial Maternal and Kid Health Officer within 14 days of the maternal days every bit stipulated.
Data quality
The quality of data is influenced by the clarity of surveillance forms, the quality of preparation and the supervision of persons who complete the maternal death notification forms and the amount of care that is exercised in managing the surveillance information. A review of these features of a surveillance organisation provided an indirect measure out of the quality of information. MDNF were reviewed to bank check for completeness of the notification forms. Also, the qualifications of the people who behave maternal death audits were checked.
Sensitivity
The sensitivity of a surveillance arrangement can be assessed by the proportion of cases detected by the surveillance organization. This attribute was assessed past asking key respondents the number of maternal deaths that were picked by the MDSR system, through verifying whether maternal deaths were correctly classified.
A 1–five Likert scale was used to measure out the level of knowledge among healthcare workers. Good was a score of 4–5, fair existence a score of 3 and poor for a 0–2 score. Respondents' knowledge was assessed through existence able to correctly define the acronym MDSR, noesis of the correct reporting timeliness for a maternal expiry, knowledge of the flow of information in the MDSR system among others. A likert scale was used because information technology is very quick, like shooting fish in a barrel to run, analyse and describe conclusions based on the responses from respondents.
Ethical considerations
Permission to carry out the study was sought from the Institutional Review Board of Matabeleland North Province and Health Studies Function. The purpose of the report was explained, and confidentiality assured. Informed written consent with a portion to sign on the questionnaire was sought from written report participants and assurance of anonymity and confidentiality was given.
Results
From the calculated sample size of 39 respondents, we were able to recruit 36 participants for our study yielding a 92.3% response rate. Of the 36 health workers interviewed 26 (72.2%) were female. More than than one-half of the respondents were midwives xx (55.4%), and the other health workers contributed 16 (44.six%). The majority of the respondents 20 (55.6%) were working in government health facilities while rural district council facilities provided 9 (25.0%) and the rest 7 (19.4%) were from the mission, private and urban local authorities. The median years of service for respondents were 10 years (Q1 = 8 years, Qiii = xi.5 years) while the median age of respondents was 36 years (Q1 = 34 years, Q3 = twoscore years) [Table 1].
Reasons for tardily notification of maternal deaths
Poor wellness worker knowledge on the maternal death surveillance and response system was cited past 24 (66.7%) of the respondents. One-half of the respondents eighteen (50%) also highlighted that the lack of training on the MDSR system was some other reason for belatedly notification of maternal deaths in the district. Unavailability of guidelines and maternal death notification forms too every bit lack of cognition on the flow of information in the surveillance organisation were reported equally other reasons by 10 (27.8%) and 12 (33.3%) respectively [Table 2]. Information on the lack of guidelines at the facilities was collaborated by the PMCHO. Triangulation of information regarding the availability of guidelines was done through key informants at commune level.
Cognition of the surveillance organization
The majority of respondents 23 (63.9%) reported that they have never notified a maternal death earlier. The notification of a maternal death is the responsibility of the attention nurse. Thirty–three (94.3%) of respondents were able to country that a maternal death should be reported within 24 h to the side by side level. Half of the respondents 17 (47.2%) correctly reported that iii maternal expiry notification forms (MDNF) are completed when notifying a maternal death. The majority of respondents 34 (94.4%) reported that an MDNF should exist completed within 7 days of the occurrence of a maternal death. The overall knowledge of wellness workers was fair.
Usefulness of the MDSR organisation
Almost all the respondents 33 (91.7%) confirmed that MDSR data was existence used at their level. The majority of the respondents, 22 (61.i%) reported that they use MDSR information to provide better information for action and monitoring improvements in maternal wellness while 20 (55.6%) used the MDSR data to quantify and determine the causes and avoidance of maternal deaths in the district. A bulk of respondents 31 (86.1%) reported that they had taken decisions based on MDSR information (Table 3). There was prove of utilisation of MDSR information in the district; facilities were able to produce minutes and maternal expiry audit reports.
On activity taken based on MDSR data 26 (72.2%) of the respondents mentioned that they used MDSR data for strengthening health intendance system in early on identification of at take a chance and refer them urgently. Also, 21 (58.8%) stated that they use data for increasing community and institutional awareness of maternal mortality. Respondents 33 (91.vii%) were of the opinion that the MDSR system is useful in Hwange Commune [Tabular array 3]. The usefulness of the MDSR system was evident as the facilities had charts and graphs stuck on the walls for all to run across, the charts and graphs were for all facilities seen, they were displaying data on maternal health e.g. number of live births recorded at the facility, maternal deaths recorded at the same facility in a given time frame. These charts were targeting wellness care workers, the local community every bit well as anyone interested in maternal health.
Simplicity of the MDSR system
Only 13 (36.one%) respondents had previously completed an MDNF. Out of these 9 had never faced challenges in completing the MDNF. The bulk of the respondents stated that they commonly took more than than 15 min to complete the MDNF. Nearly all the respondents 33 (91.7%) felt that there was a need for grooming in the completion of the MDNF.
Acceptability of the MDSR arrangement
All participants felt that it was their responsibility to complete the MDNF and they were willing to keep participating in the MDSR organisation. Almost 78% (n = 28) reported that MDSR data was analysed and 15 (55.6%) were able to produce reports equally evidence of data analysis. Xx-one (60.0%) reported having held maternal decease inspect meetings at their facilities. Reports on the audit meetings held at facilities were availed.
Stability of the MDSR organisation
The majority of respondents 30 (83.iii%) interviewed were non trained in MDSR, but six reported having received training. Those that were trained received preparation in the form of on the task training and workshop grooming. 5 out of eleven health facilities had maternal death notification forms, and they were acceptable. But two facilities out of 11 (18.2%) had maternal decease instance definitions, and the definitions were kept on a shelf and not displayed. All 11/eleven (100%) facilities had a phone for communication with adjacent level of intendance. Four out of 11(36.4%) wellness facilities were constitute with maternal death audit guidelines [Table 4].
The cost of completing three MDNF and submitting them to the district office was calculated. Bold that the health worker completing the form earned a monthly salary of $500, 20-2 working days per month and an viii-hour working 24-hour interval. The price of transporting an MDNF @ $0.31/km was $57.04. Nosotros used the furthest wellness facility from the district office (Kamativi clinic). The total cost of running the MDSR system in Hwange district was $lx.78 [Table five].
Discussion
All the deaths recorded in the commune were institutional deaths, no customs deaths were recorded. This could be as a issue of lack of a functional arrangement for routinely identifying maternal deaths in the community. There is a likelihood of deaths occurring in the customs simply because at that place is no way of capturing and recording these deaths, they may be going unnoticed. This important finding concurs with findings fabricated by Moodley et.al in Southward Africa where they emphasised that maternal death enquiries are facility based with no system currently for routinely identifying deaths in the community [sixteen]. Our findings are in contradiction with the WHO'southward recommendations on community participation in MDSR which emphasises the importance of sharing information on pregnancy related deaths with communities including word of different factors causing these deaths and affecting access to skilled care [17].
Lack of information sharing between health care workers and communities creates a huge gap and after pregnancy related problems affecting the same communities are not given the attending they deserve. Another study done in Sierra Leone revealed that at community level the notification and reporting of maternal deaths was one of the biggest challenges identified. The customs failed to written report maternal deaths considering of numerous socio cultural reasons. The study also revealed that maternal deaths did occur but were not reported because of fearfulness of repercussions by community members. This might besides be one of the contributing factors for not recording community deaths in Hwange district.
Our study results revealed that wellness workers in Hwange district had off-white knowledge on the MDSR. Lack of acceptable noesis on the MDSR system meant that health workers had little idea of what was expected from them. This gap in knowledge fuels further delays in the maternal death notification process. Furthermore, lack of acceptable cognition on the MDSR allows for many deaths, maternal or otherwise to become unrecorded or are incorrectly classified which results in underreporting of maternal mortality. Every misclassified or unrecorded maternal expiry is a lost opportunity to take cosmetic action to ensure that other women do non die in the same way [18].
Our written report also found some inconsistencies from health workers with regards to the number of maternal expiry notification forms that are completed when notifying a maternal death, one-half of the health workers correctly mentioned iii forms, and the other reported that 4 maternal expiry notification forms are completed. Such inconsistencies are a clear indication that wellness workers in the district lack adequate knowledge of the surveillance system. The inconsistencies can be attributed to the fact that about of the maternal deaths recorded occurred in the infirmary setting and the notification process was only confined to those health workers in the district hospital thereby excluding those wellness workers in the rural health facilities. These findings are consequent with findings made by Mutsigiri at.al in Mutare district where they reported that well-nigh maternal deaths occurred at the commune or provincial hospitals hence only health workers at these referral facilities were exposed to the surveillance system and thereby excluding those at the rural health facilities [xix].
We also plant that wellness workers were able to correctly state the correct timelines for the notification of a maternal death to the next level. All the same, even with this noesis of timelines, Hwange commune was notifying maternal deaths late. Lack of preparation on the surveillance system coupled with the unavailability of notification forms at the wellness facilities were reasons cited by most health workers for notifying maternal deaths late. Inadequate human resource were too cited every bit another reason for late notification of maternal deaths in Hwange district. The district had three doctors practicing however we managed to recruit merely ane medical doctor, this is because the district is seriously brusk staffed and the dr. was the but one available at the fourth dimension of data collection. Like findings were as well made by Mutsigiri et al., where they highlighted that maternal deaths were not reported on time because health workers encountered as well much workload and a shortage of staff. Timely reporting of a maternal decease improves the accurateness of information obtained and underscores the benefits of making a maternal death a notifiable event [18]. Timely notification of maternal deaths, assessment and confirmation of cases, increased awareness and advocacy adds value to active surveillance of maternal deaths [eighteen].
Our report revealed that there was a need for training of healthcare workers in the completion of the MDNF, the majority of the health workers had never completed an MDNF before therefore respondents felt that they were inadequately prepared in the outcome a maternal decease occurs at their facility. This training gap is considering in rural health facilities maternal deaths are rare events so this explains why most health workers have never completed an MDNF before. These findings are consistent with findings made past Chirundu et al. (2017) in Sanyati district where they reported that only 24% of respondents reported having completed an MDNF before. Training of health workers in MDSR give them a practical approach to maternal health and too boost their knowledge of the MDSR organisation. This grooming of health care workers on MDSR will, therefore, equip them to have a better reporting arrangement which will capture disquisitional information that will inform targeted approaches to improve maternal health care [20]. The cognition gap fuels underreporting and poor use of MDSR data, this, in turn, makes data inappropriate for proactive response, planning and resource allotment [21].
We also found that facilities in Hwange had no maternal death case definitions and the few that had the case definitions kept them on the shelves, and they were not displayed for all to encounter and use. Keeping maternal example definitions on the shelves may exist a sign that these definitions are not being used at all in these facilities. Example definitions act as refresher material for health workers, and they aid in the proper classification of a maternal death when it happens. These definitions are office of a strategy for the improvement of the quality of maternal wellness intendance, which will ideally, lead to a reduction of maternal morbidity and mortality [20].
The usefulness of the MDSR system was evident in Hwange district; there was evidence of the utilise of data on the surveillance system through the production of facility reports as well as wall charts with data such every bit graphs and statistics. The acceptability of the MDSR arrangement amongst health workers was reportedly loftier; this is however non a true reflection of the actual performance of the MDSR arrangement in Hwange. Health workers are aware of their daily responsibilities and their mandate to study maternal deaths on time, so many of them are likely to report a willingness to continue participating in the MDSR system.
The stability of the MDSR system was affected by lack of grooming and or induction of health workers on the surveillance system, unavailability of case definitions, unavailability of the notification forms as well as unavailability of maternal death inspect guidelines at facilities. These resource when in brusque supply trigger the inability of health systems to measure levels and trends in maternal mortality reliably, this contributes to lack of accountability and in turn lack of progress in achieving the goal of reducing maternal mortality through the implementation of the MDSR organisation [22]. Almost all facilities had a functional computer and a printer for producing textile that is needed in the surveillance system. Nonetheless very few of the institutions had an internet connexion. Facilities ought to have access to applied science so that health workers can access information regarding maternal health whenever they need it.
Our written report had some limitations. Most of the information obtained was subjectively assessed; however, some evidence to back up the findings was obtained from the facility records (reports and minutes). We were too unable to examine all the system attributes due to non availability of data on the attributes. However we objectively assessed some of the attributes hence this study provides useful information on the performance of the maternal decease surveillance and response system in Hwange commune.
Conclusions
We ended that in Hwange district, the MDSR arrangement is useful, adequate, flexible and somewhat stable. The system is nonetheless costly and not uncomplicated to utilize by health workers. Reasons for tardily notification of maternal deaths were lack of adequate knowledge of wellness care workers on the MDSR organization and lack of proper induction on the MDSR in the district. We recommend induction or orientation of all health workers involved in MDSR, Standard Operating Procedures on the completion of maternal expiry notification forms to be availed to health workers in health facilities. As a consequence of this study, a soft copy of the latest maternal expiry notification form was distributed to those wellness facilities that did non have an MDNF. Likewise, copies of the maternal decease audit guidelines were sourced and distributed to all health facilities.
Abbreviations
- CDC:
-
Centers for Illness Control and Prevention
- DHIS two:
-
District Health Data Arrangement ii
- MDG:
-
Millennium Development Goals
- MDNF:
-
Maternal Death Notification Class
- MDSR:
-
Maternal Death Surveillance and Response
- MMSR:
-
Maternal Mortality Surveillance and Response
- WHO:
-
World Health Organisation
References
-
IDSR Technical Guidelines 2nd Edition_2010_English.pdf [Cyberspace]. [cited 2017 Jun 29]. Available from: https://www.cdc.gov/globalhealth/healthprotection/idsr/pdf/technicalguidelines/idsr-technical-guidelines-2nd-edition_2010_english.pdf.
-
UNICEF, editor. Maternal and newborn wellness. New York, NY: UNICEF; 2008. 158 p. (The state of the world'southward children).
-
WHO | International Classification of Diseases [Internet]. [cited 2017 Jun 29]. Available from: https://www.who.int/classifications/icd/en/.
-
Globe Health Arrangement, UNICEF, United Nations Fund for Population Activities, World Bank, Un, Section of Economic and Social Diplomacy, et al. trends in maternal bloodshed, 1990 to 2013: estimates by WHO, UNICEF, UNFPA, the World Depository financial institution estimates, and the United nations Population Partition [Internet]. 2014 [cited 2017 Jun 29]. Available from: https://apps.who.int/iris/bitstream/handle/10665/112697/WHO_RHR_14.13_eng.pdf;jsessionid=E659BDE875532EE3EB043C9763173D66?sequence=1.
-
WHO | Maternal deaths vicious 44% since 1990 – UN [Internet]. WHO. [cited 2017 Sep 26]. Available from: https://www.who.int/en/news-room/detail/12-11-2015-maternal-deaths-fell-44-since-1990-un.
-
WHO | Maternal mortality [Cyberspace]. WHO. [cited 2017 Jun thirty]. Available from: http://www.who.int/gho/maternal_health/mortality/maternal_mortality_text/en/
-
drroopesh. "Globe Health Statistics 2016: Monitoring Health for the SDGs" Released! (xix May 2016) [Net]. communitymedicine4asses. 2016 [cited 2017 Jun thirty]. Bachelor from: https://communitymedicine4asses.wordpress.com/2016/05/20/world-health-statistics-2016-monitoring-health-for-the-sdgs-released-nineteen-may-2016/
-
Organization WH. World wellness statistics 2016: monitoring wellness for the SDGs sustainable development goals, vol. 131: World Health Organisation; 2016.
-
Temmerman M, Khosla R, Laski L, Mathews Z, Say 50. Women's health priorities and interventions. BMJ 2015 Sep xiv;351:h4147.
-
WHO Perspectives on Maternal Mortality in Zimbabwe: A Reflection of the Twelvemonth 2014 [Internet]. [cited 2017 Jul three]. Available from: http://www.afro.who.int/republic of zimbabwe/press-materials/detail/7271-who-perspectives-on-maternal-mortality-in-zimbabwe-a-reflection-of-the-yr-2014.html?lang=en
-
WHO | MDG 5: improve maternal health [Cyberspace]. WHO. [cited 2017 Jul 5]. Available from: http://www.who.int/topics/millennium_development_goals/maternal_health/en/
-
WHO | Maternal Death Surveillance and Response - groundwork [Internet]. WHO. [cited 2017 Oct 9]. Available from: http://world wide web.who.int/maternal_child_adolescent/epidemiology/maternal-decease-surveillance/groundwork/en/
-
Abouchadi South, Belghiti Alaoui A, Meski FZ, De Brouwere 5. Implementing a maternal mortality surveillance arrangement in Morocco–challenges and opportunities. Tropical Health International Medicine 2013; eighteen (3): 357–365. pmid:23289440.
-
Centers for Illness Control (CDC). Guidelines for evaluating surveillance systems. MMWR Suppl. 1988;37(5):ane–xviii.
-
gtr_casestudy_mexico_eng.pdf [Internet]. [cited 2017 Jul 5]. Available from: https://www.msh.org/sites/msh.org/files/gtr_casestudy_mexico_eng.pdf
-
Updated Guidelines for Evaluating Public Wellness Surveillance Systems [Internet]. [cited 2017 Jul 5]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5013a1.htm
-
http://www.who.int/maternal_child_adolescent/documents/9241591838/en/
-
Scott H, Dairo A. Maternal Death Surveillance and response in east and southern Africa. J Obstet Gynaecol Can JOGC J Obstet Gynecol Can JOGC. 2015;37(10):915–21.
-
Mutsigiri-Murewanhema F, Mafaune PT, Juru T, Gombe NT, Bangure D, Mungati M, et al. Evaluation of the maternal mortality surveillance organization in Mutare district, Zimbabwe, 2014-2015: a cross sectional study. Pan Afr Med J [Internet]. 2017 Jul 18;27. Bachelor from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5579423/.
-
UNFPA Pacific Sub-Regional Office -- Maternal health care surveillance preparation boost for Solomon Islands [internet]. [cited 2017 Jul 5]. Bachelor from: http://countryoffice.unfpa.org/pacific/2016/10/05/14154/maternal_health_care_surveillance_training_boost_for_solomon_islands/.
-
Abouchadi S, Shahabuddin A, Zhang WH, Firoz T, Englert Y, Nejjari C, et al. Existing models of Maternal Decease Surveillance systems: protocol for a scoping review. JMIR Res Protoc [Internet]. 2016 Oct xi;5(4). Bachelor from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5080526/
-
WHO | Maternal death surveillance and response [Cyberspace]. WHO. [cited 2017 Jul 5]. Available from: http://www.who.int/message/volumes/89/11/11-097220/en/
Acknowledgements
I would similar to express my sincere gratitude to the District Wellness Executive of Hwange, Provincial Health Executive of Matabeleland North for their unwavering support. I would besides like to limited my gratitude to the MPH colleagues, Department of Customs Medicine, University of Republic of zimbabwe and the Health studies Office, Republic of zimbabwe for all the back up. Finally I would similar to thank my loving married woman Beryl for the support throughout the report.
Funding
The report was funded past Centres for Disease Command and prevention (CDC).
Availability of information and materials
The datasets generated and/or analysed during the current study are available from the respective author on reasonable asking.
Writer information
Affiliations
Contributions
MM1, NM: formulation and design of report, data collection and analysis, drafting the manuscript. TJ: formulation and design of study, reviewing several drafts of the manuscript for of import intellectual content. MM2, MT, NG, PN: Formulation and design of study and critically reviewing the manuscript for important intellectual content. All authors read and approved the final manuscript for publication.
Corresponding writer
Ethics declarations
Ethics approval and consent to participate
Permission to carry out the study was sought from the Institutional Review Lath of Matabeleland Due north Province and Health Studies Role. The purpose of the study was explained, and confidentiality bodacious. Informed written consent with a portion to sign on the questionnaire was sought from study participants and assurance of anonymity and confidentiality was given.
Consent for publication
"Not applicable".
Competing interests
The authors declare that they have no competing interests.
Publisher'south Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the information made bachelor in this commodity, unless otherwise stated.
Reprints and Permissions
Almost this article
Cite this article
Maphosa, Yard., Juru, T.P., Masuka, N. et al. Evaluation of the Maternal Expiry Surveillance and response system in Hwange District, Zimbabwe, 2017. BMC Pregnancy Childbirth 19, 103 (2019). https://doi.org/ten.1186/s12884-019-2255-1
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12884-019-2255-1
Keywords
- Evaluation
- Maternal Death Surveillance and response
- Hwange
- Zimbabwe
Source: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-019-2255-1
0 Response to "Existing Models of Maternal Death Surveillance Systems Protocol for a Scoping Review"
Post a Comment